Reassessing the Role of Intravenous Albumin in Modern Medicine
Category: Modern Medicines
Date: 2025-08-13
A Deep Dive into the Latest International Guidelines
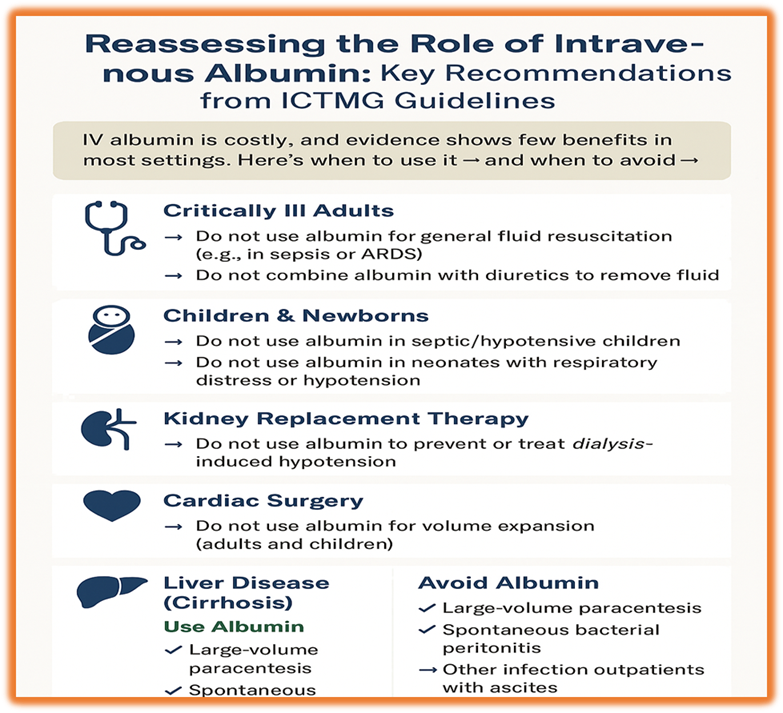
Albumin infusion has long held a privileged position in hospital care, viewed by many clinicians as a powerful tool for stabilising critically ill patients, managing cirrhosis complications, and preventing dialysis-induced hypotension. But a comprehensive 2024 guideline published in CHEST by the International Collaboration for Transfusion Medicine Guidelines (ICTMG) has taken a bold step—it urges the global medical community to rethink how, when, and even if albumin should be used.
This guideline, formulated through a meticulous review of randomised controlled trials (RCTs) and systematic reviews, provides 14 evidence-based recommendations, challenging many conventional uses of albumin and promoting a more judicious, targeted approach.

🔍 Why This Guideline Matters
Albumin is a blood-derived, high-cost product, often administered without strong supporting evidence. Many clinicians equate low serum albumin with a need for infusion, or use it in hypotensive or fluid-overloaded patients under the belief that it provides a "superior" fluid resuscitation alternative to crystalloids.
But what does the science say?
The ICTMG guidelines evaluated the clinical benefits, harms, costs, and outcome relevance across six key patient groups:
- Critically ill adults
- Critically ill children and neonates
- Kidney replacement therapy recipients
- Cardiovascular surgery patients
- Cirrhosis and liver disease populations
- Outpatients with complications of ascites
📋 Key Findings: What the Guidelines Recommend
1. 🏥 Critically Ill Adult Patients
- Do not use albumin as a first-line fluid resuscitation in critically ill patients (including sepsis, ARDS, or trauma).
- Albumin combined with diuretics does not improve fluid removal or clinical outcomes.
- Even in thermal injuries or ARDS, no meaningful benefits were found with albumin.
➡️ Rationale: Large RCTs and meta-analyses, including over 20,000 patients, found no mortality benefit with albumin versus crystalloids. Albumin may increase harm in subgroups like traumatic brain injury.
2. 👶 Paediatric and Neonatal Populations
- Children with infection or hypoperfusion: Albumin does not reduce mortality and may be harmful.
- Neonates (especially preterm): Albumin does not improve respiratory function, circulation, or survival.
➡️ Rationale: The landmark FEAST trial (3,000+ children in Africa) showed increased mortality with both albumin and saline boluses compared to no bolus at all. Neonatal trials showed no significant benefits in any outcome.
3. 🩺 Patients on Dialysis or Kidney Replacement Therapy
- Albumin is not recommended to prevent or treat intradialytic hypotension or to improve ultrafiltration.
➡️ Rationale: Evidence from small RCTs showed that while BP may transiently improve, no consistent benefit in dialysis adequacy, morbidity, or long-term outcomes was seen. The cost is exceptionally high, up to $20,000/year per patient.
4. ❤️ Cardiovascular Surgery
- Adults and children undergoing bypass surgery should not receive albumin for priming or volume expansion.
➡️ Rationale: Among nearly 4,000 surgical patients studied, albumin did not reduce blood loss, ICU stay, infection, or mortality. In fact, a major trial reported higher rates of bleeding and infection with albumin.
5. 🧬 Cirrhosis and Liver Disease
Here’s where albumin finds limited, but targeted use:
✅ Recommended (conditionally):
- Large-volume paracentesis (>5 L): Albumin helps prevent circulatory dysfunction.
- Spontaneous bacterial peritonitis (SBP): Albumin reduces mortality and kidney injury.
❌ Not recommended:
- Routine use in hospitalised cirrhotic patients with low albumin.
- Extraperitoneal infections (e.g., pneumonia or UTI).
- Outpatients with stable ascites not requiring frequent paracentesis.
- Correction of serum albumin alone (<30 g/L) without other indications.
➡️ Rationale: Although albumin may reduce post-paracentesis complications or aid in SBP outcomes, the evidence quality is low, and several studies report fluid overload, pulmonary edema, and increased hospital burden.
💰 The Economics of Albumin: Is It Worth It?
IV albumin is significantly more expensive than crystalloids. Despite its cost:
- It does not improve survival in critical illness.
- It does not reduce kidney failure risk in dialysis.
- It does not shorten hospital stays in cardiac or liver patients.
The routine use of albumin not only burdens healthcare budgets but also increases the risk of adverse effects, including volume overload, allergic reactions, and unnecessary transfusion exposure.
🔮 What Does the Future Hold?
Currently, 5 large clinical trials are underway investigating albumin in:
- Septic shock
- Cardiac surgery
- Acute kidney injury
- Outpatient cirrhosis care
- Pneumonia-related hospital admissions
These studies will likely redefine the role of albumin in specific, high-risk subgroups. Until then, this guideline encourages clinicians to limit albumin use to:
- Paracentesis-related circulatory dysfunction
- SBP with cirrhosis and risk of kidney failure
Every other use should be individualised, supported by evidence, and weighed against cost and harm.
🧠 Final Thoughts: A Shift from Habit to Evidence
This 2024 guideline represents a paradigm shift. Albumin, once liberally used, is now being called into question. The message is clear:
"Don’t treat numbers. Treat the patient. And use albumin only when it helps—not just because it’s available."
Let’s move towards value-based, evidence-guided care that ensures better outcomes, lower costs, and reduced unnecessary interventions.

